Complete Clinical Path and Technical Analysis of Artificial Insemination
Artificial Insemination (AI) is an assisted reproductive technology in which processed semen is injected directly into the female reproductive tract (mainly intrauterine insemination) through non-coital means. The core principle is to increase the probability of sperm meeting the egg by optimizing the path and timing of sperm delivery. Depending on the source of sperm, it is categorized into artificial insemination by husband (AIH), which is suitable for men with mild to moderate oligozoospermia or sexual dysfunction, and artificial insemination by donor (AID), which is for couples with azoospermia or a high risk of genetic disorders. Compared to In Vitro Fertilization (IVF), the advantages of AI are that it is easy to perform (on average, it takes 15 minutes), inexpensive (the cost of a single cycle is about 1/10 of that of IVF), and closer to the physiological process of natural pregnancy.
Stage 1: Rigorous medical evaluation (1-30 days)
Prior to initiating treatment, the patient completes a systematic medical evaluation to rule out contraindications and optimize the conditions for pregnancy:
Female Fertility Assessment
Ovarian reserve function: Ovarian responsiveness is assessed by anti-Müllerian hormone (AMH) testing (threshold ≥ 1.1 ng/mL) and sinus follicle count (AFC ≥ 5).
Tubal patency: hysterosalpingography (HSG) was preferred, with referral for laparoscopy or direct IVF if bilateral obstruction was demonstrated.
Uterine environment: transvaginal ultrasound to measure endometrial thickness (≥7 mm at ovulation is ideal), and hysteroscopy to rule out polyps or adhesions if necessary.
Male semen analysis
Criteria for semen optimization: After processing by density gradient centrifugation, the total number of forward-moving spermatozoa needs to be ≥5×10⁶ and the DNA fragmentation index (DFI) <30%. For patients with severe oligospermia (e.g., total motile sperm <1×10⁶), it is recommended to upgrade to ICSI technology. Frozen semen processing: the donor specimen should be quick-frozen in liquid nitrogen (cooling rate -20°C/min) and resuscitated in a 37°C water bath, and the survival rate should be >50%.
Genetics and infection screening
Compulsory tests include karyotyping, genetic testing for thalassemia, and screening for infectious diseases such as HIV, hepatitis B and syphilis. For sperm donor cycles, matching of blood type and phenotypic characteristics is also required.
Phase 2: Individualized Ovulation Management (Natural Cycle/Ovulation Promotion Cycle)
Natural cycle monitoring (days 8-14 of menstruation)
Follicle tracking: Starting on day 8 of menstruation, follicular development is monitored by transvaginal ultrasound every 48 hours, focusing on sinus follicles with a diameter of 10-12 mm. When the dominant follicle reaches 14 mm, the monitoring is changed to daily.
Hormonal dynamics assessment: synchronized serum LH, estradiol (E2) and progesterone (P) were measured, with peak LH >25 IU/L suggesting impending ovulation.
Insemination timing decision: 24-36 hours after the appearance of LH peak or when the follicle diameter is ≥18 mm, hCG injection of 5,000-10,000 IU triggers ovulation, and artificial insemination is performed within 12-36 hours after the injection.
Ovulation induction cycle program (days 3-12 of menstruation)
Drug of choice:
Clomiphene (Clomiphene): 50 mg/d (days 3-7 of menstruation), induces FSH secretion by antagonizing estrogen receptors, but may increase risk of endometrial thinning (incidence 15%).
Letrozole (Letrozole): 2.5 mg/d (days 3-7 of menstruation), promotes follicular recruitment by elevating androgen levels in the ovary through inhibition of aromatase, especially in patients with polycystic ovary syndrome (PCOS).
Follicular response monitoring:
Ultrasound monitoring is initiated on day 8 of menses and alerts to the risk of multiple pregnancies when ≥2 follicles ≥14 mm in diameter are present (incidence 8%-12%).
Dynamically adjust GnRH antagonist (e.g. Cetrotide 0.25 mg/d) to prevent early onset LH peak and maintain synchronized follicular development.
Phase III: Refined insemination operation (critical 24 hours)
Semen processing techniques
Gradient centrifugation: Use 40%-80% density gradient solution to separate high viability spermatozoa, remove prostaglandins and immune factors from seminal plasma, and control the processing time within 30 minutes to avoid oxidative damage.
Sperm activation: Addition of culture medium containing calcium ion carriers (e.g. A23187) to induce sperm acrosome reaction and improve penetration of the zona pellucida of the egg.
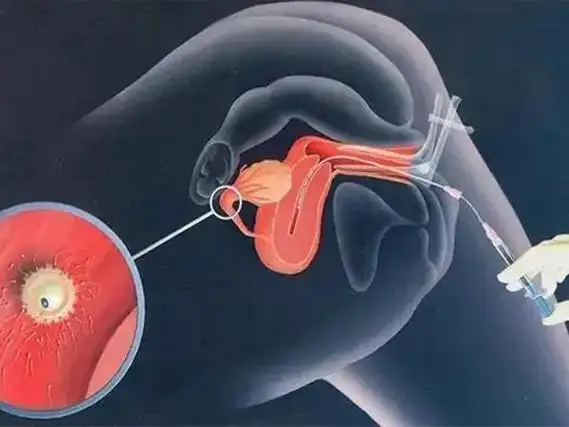
Intrauterine insemination (IUI) operation
Catheter selection: Preference is given to the use of soft catheters (e.g. Wallace®) with a bend that adapts to the angle of the cervix and reduces endothelial trauma (bleeding rate <3%).
Sperm suspension injection: 0.3-0.5 mL of suspension containing ≥5×10⁶ forward-moving spermatozoa is slowly injected into the proximal uterine cavity, and the supine position is maintained for 15 minutes after the procedure to promote sperm migration.
Double insemination strategy: one IUI at 24 hours and one at 48 hours after hCG injection has been shown in clinical data to enhance pregnancy rates to 18%-22%.
Stage 4: Luteal Support and Early Pregnancy Management (15-30 days)
Luteal Function Reinforcement
Progesterone supplementation program:
Vaginal gel (Crinone 8%): once daily, utilizing the uterine first-pass effect to achieve local endometrial concentrations up to 100 times that of serum.
Oral dextroprogesterone: 10 mg bid, its metabolite DHD selectively binds to progesterone receptors and reduces systemic side effects.
Adjunctive hCG: In patients with luteal insufficiency (P < 10 ng/mL after ovulation), inject hCG 1,500 IU every 3 days to maintain luteal activity. Pregnancy Confirmation and Monitoring Serum β-hCG test: 14 days postoperatively, threshold ≥50 IU/L suggests biochemical pregnancy and needs to be repeated after 48 hours to confirm multiplication (increase >66% is normal).
Early ultrasound evaluation: transvaginal ultrasound at 5 weeks of gestation to confirm the location of the gestational sac and fetal heartbeat, and to exclude ectopic pregnancy or embryonic arrest.
Stage 5: Cycle outcome analysis and strategy optimization
For successful pregnancy: continue luteal support until 10-12 weeks of gestation and gradually reduce and stop the drug. For multiple pregnancies (incidence 5%-8%), fetal reduction at 11-13 weeks of gestation is required to minimize obstetric risk.
Failure to conceive:
Reason for failure analysis: potential problems are localized by semen parameter review, tubal patency reassessment, and endometrial receptivity assay (ERA).
Protocol adjustment: if 3 consecutive cycles are infertile, switching to IVF treatment is recommended; for patients with repeated implantation failure (RIF), endometrial scratching or immunomodulatory therapy may be attempted.
Factors affecting success rate and coping strategies
Age correlation: the cumulative pregnancy rate of women under 35 years old can reach 40%-50%, while it drops to 8%-12% for those over 40 years old, so it is recommended to choose IVF directly for patients of advanced age.
Sperm quality threshold: pregnancy rates plummet to less than 5% with forward-moving sperm <5×10⁶, requiring combined sperm optimization techniques (e.g., IMSI) or testicular sperm extraction (TESE).
Psychological interventions: anxiety and depressive states can reduce pregnancy rates by up to 30%, and cognitive behavioral therapy (CBT) and positive thinking training can improve endocrine homeostasis.
The success of artificial insemination, the cornerstone technology of the assisted reproduction system, relies on precise individualized protocol design, rigorous laboratory quality control, and interdisciplinary collaboration. With the popularization of technologies such as microfluidic sperm sorting and AI ovulation prediction, the cycle pregnancy rate of AI is expected to exceed 30% in the future, providing more families with efficient and safe fertility solutions.
相关推荐
- 2025 Ultimate Guide to IVF in Three Central Asian Countries: Georgia, Kazakhstan, and Kyrgyzstan
- The Three Golden Rules of IVF Success
- Luteal support for 144 hours: a new discovery on the golden window to improve IVF success rate
- Endometrial tolerance is the invisible key to IVF failure
- Seven Differences Between IVF and Natural Pregnancy
Search within the site
Surrogacy News
Hot Tags.
Kyrgyzstan Surrogacy Agency,Global IVF Hospitals,International Surrogate Mother Recruitment